The Link Between Sleep and Chronic Pain
Good sleep is hard to come by during this pandemic. The impossible juggle of work, kids at home, stress and isolation has challenged sleep for many. We know that poor sleep has a huge impact on many aspects of physical and mental health, and recent research also shows a relationship between sleep disturbances and chronic pain. According to Maslow, sleep is one of our basic physiological needs. Unfortunately, sleep is often regarded as an optional luxury rather than an essential pillar of health. This article explores the impact of sleep on chronic pain, and we share our top “sleep hygiene” tips for a more restful night’s sleep.
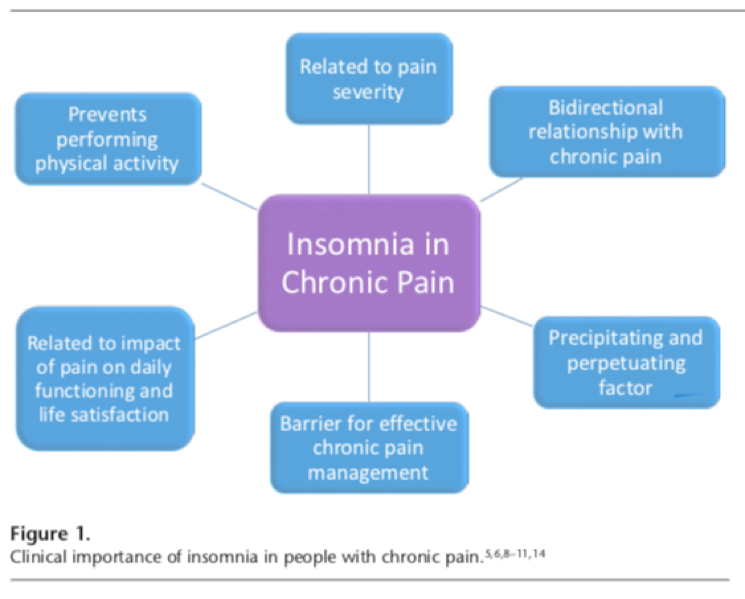
Sleep and Chronic Pain
A recent review article by Nijs and co-authors1 beautifully summarises how sleep can influence chronic pain, and discusses the impact on central sensitisation, neuroinflammation and more. We have summarised a few of these interesting insights below:
Sleep and Central Sensitisation
There is a close association between sleep problems and central sensitisation. Many studies have found that sleep disturbances lead to hyperexcitability of the central nervous system (CNS) and lowering of the pain threshold. For example, a single night of sleep deprivation has been found to increase hyperalgesia and anxiety in healthy people1. A reduction in sleep has also been found to impact endogenous nociceptive-inhibitory function and increase pain in healthy people1. It is likely that a vicious cycle exists, with poor sleep leading to lower pain thresholds, which contributes to hyperalgesia, which in turn worsens sleep quality1.
Sleep and Development of Widespread Pain
A longitudinal study from Sweden of nearly 1000 men and women investigated whether insomnia is a risk factor for local pain developing into widespread pain. They found a strong prospective relationship that people with local pain and insomnia were more likely to develop widespread pain than those without insomnia2.
Sleep and Neuroinflammation
While healthy sleep promotes immune function, sleep disturbances can result in low grade CNS inflammation1. Poor sleep leads to an increase in inflammatory cytokines, which affect brain function, interfere with CNS-meditated fatigue, and correlate with increased pain sensitivity1.
Source: Nijs, J., Mairesse, O., Neu, D., Leysen, L., Danneels, L., Cagnie, B., Meeus, M., Moens, M., Ickmans, K. and Goubert, D. (2018). Sleep Disturbances in Chronic Pain: Neurobiology, Assessment, and Treatment in Physical Therapist Practice. Physical Therapy, 98(5), pp.325-335.
If you want to learn more about sleep disturbances and the impact on pain, this article is a must read.
Sleep Hygiene Tips
The National Sleep Foundation recommends adults sleep 7-9hrs each night.
If your patients are not getting enough sleep, some of these simple “Sleep Hygiene” tips might help:
- Keep stimulants such as caffeine, nicotine and alcohol to a minimum. The most important time to minimise these are 4-6 hours before bed.
- Avoid naps during the day, and especially not after 3pm.
- Get into a routine: getting up at the same time each morning and going to bed at the same time each night (even on the weekend) improves the quality of your sleep.
- Have a buffer zone of 1-2 hours between any stimulating evening activities and going to bed. During this wind-down time turn off computers and electronic devices. Light from these devices suppresses melatonin and will affect sleep.
- Undertake relaxing activities like watching pleasant TV programs, reading, listening to music, chatting, reading magazines, having a warm bath or shower, or drinking a warm non-caffeinated, non-alcoholic drink. Have hot milk before bed - a brain trigger for sleep.
- Keep your bedroom cool: around 18° is optimal for most people.
- Don’t spend your day in your bedroom etc. studying or watching TV – bedroom is for sleep and intimacy only.
- If you are lying awake feeling frustrated, then get out of bed and do something relaxing until you feel more ready for sleep. Keep the lights dim.
- If you wake up in the middle of the night, don’t turn on your screen – read, stretch, focus on your breathing or even try and contract and relax your facial muscles in turn - this is still a form of rest.
These tips are shared on our patient blog ‘Sleep: Your Superpower’, which might be a helpful resource for your patients.
Prioritise Sleep
For any patients presenting with pain, it is recommended to routinely ask about sleep quality and quantity as a part of the assessment. You may also find it helpful to ask patients to complete a validated tool such as an Insomnia Severity Index to objectively assess the degree of their sleep issues. Addressing sleep problems can make a big difference to chronic pain, and improve many other aspects of health also. Patients need to be encouraged to make sleep a priority, and understand the positive impact better sleep can have on many aspects of physical and mental health, including pain.
References
1 Nijs, J., Mairesse, O., Neu, D., Leysen, L., Danneels, L., Cagnie, B., Meeus, M., Moens, M., Ickmans, K. and Goubert, D. (2018). Sleep Disturbances in Chronic Pain: Neurobiology, Assessment, and Treatment in Physical Therapist Practice. Physical Therapy, 98(5), pp.325-335.
2 Wiklund T, Gerdle B, Linton SJ, Dragioti E, Larsson B. Insomnia is a risk factor for spreading of chronic pain: A Swedish longitudinal population study (SwePain). Eur J Pain. 2020;00: 1–9. https://doi.org/10.1002/ejp.1582
October 2020